Image source: https://cdn.hepatitisc.uw.edu/doc/138-1/paracentesis-z-technique.jpg
Ascites is the presence of excess fluid in the peritoneal cavity. It is a common clinical finding with a wide range of causes, but develops most frequently as a part of the decompensation of previously asymptomatic chronic liver disease. The symptoms of ascites vary from patient to patient and depend largely on the quantity of fluid. If trace ascites is present, the patient may be asymptomatic, and fluid is detected only on physical or radiologic examination. If a large amount of fluid is present, the patient may complain of abdominal fullness, early satiety, abdominal pain, or shortness of breath.
Ascites is detected on physical examination of the abdomen by visible bulging of the flanks in the reclining patient ("flank bulging"), "shifting dullness" (difference in percussion note in the flanks that shifts when the patient is turned on the side) or in massive ascites with a "fluid thrill" or "fluid wave" (tapping or pushing on one side will generate a wave-like effect through the fluid that can be felt in the opposite side of the abdomen).
Rapidly developing (acute) ascites can occur as a complication of trauma, perforated ulcer, appendicitis, or inflammation of the colon or other tube-shaped organ (diverticulitis). This condition can also develop when intestinal fluids, bile, pancreatic juices, or bacteria invade or inflame the smooth, transparent membrane that lines the inside of the abdomen (peritoneum). However, ascites is more often associated with liver disease and other long-lasting (chronic) conditions.
Ascitic fluid is derived from the vascular compartment subserving the hepatosplanchnic viscera. Two factors are important in the formation of ascites: an increased total body sodium and water, and increased sinusoidal portal pressure. In cirrhosis, hepatic dysfunction and sinusoidal portal pressure probably both send a message to the kidney to retain excess sodium and fluid, while the portal hypertension serves to localize excess fluid to the peritoneal cavity rather than the periphery.
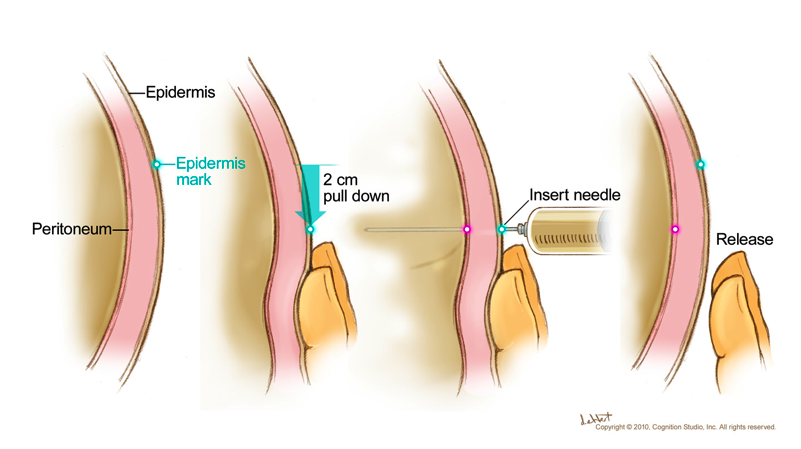
The ascitic tube (drain) is usually inserted by a doctor and the procedure can be done at the bedside in the ward or in the outpatients clinic. Sometimes the drain may be inserted in the ultrasound department whilst scanning the abdomen. This helps the doctor find exactly where to put the drain, especially if the fluid appears to be in small pockets and cannot be drained all at once. You will be asked to lie on the bed while the skin in the area where the drain is to be inserted is cleaned with an antiseptic solution, which prevents it from becoming infected.
Many patients remain asymptomatic until decompensation occurs. Lack of symptoms and minor liver enzyme elevations are typical of HCV infection and cannot be taken as evidence of lack of progression. HCV RNA testing confirms the diagnosis. Liver biopsy helps assess disease activity and stage the severity of fibrosis and is recommended for most patients with hepatitis C. Once this information is obtained, a rational program for treatment and monitoring can be planned.
Nonspecific abdominal discomfort and dyspnea may occur with massive ascites, but lesser amounts are usually asymptomatic. The diagnosis is made clinically by detecting shifting dullness on abdominal percussion, though US or CT scan can detect much smaller amounts of fluid. In advanced cases the belly is taut, the umbilicus is flat or everted, and a fluid wave can be elicited. Differentiation from obesity, gaseous distention, pregnancy, or ovarian tumors and other intra-abdominal masses usually is easily made by clinical examination, but scanning techniques or diagnostic paracentesis may occasionally be required.